Given that many people with asthma also have allergies, providers may receive questions from patients with asthma about possible allergic reactions to COVID-19 vaccines. The American Academy of Allergy, Asthma and Immunology COVID-19 task force is providing updates on the recommendations and research. In short, at this point, the recommendations are as follows:
- All COVID-19 vaccines should be administered in a facility where each person can be monitored for at least 15 minutes with treatment readily available for anaphylaxis. Anyone with a history of non-anaphylactic reactions to food, oral medication, latex, environmental, or venom allergens can safely receive either the Pfizer or Moderna vaccine in this manner.
- Anyone with a history of anaphylaxis to food, oral medication, latex, environmental, or venom allergies can receive either the Pfizer or Moderna vaccine without any precautions other than a recommended 30-minute observation period.
- Anyone with a history of immediate onset hypersensitivity reactions (urticaria, wheezing, angioedema, anaphylaxis) to any prior vaccine or injected medication can receive either the Pfizer or Moderna vaccine with a recommended 30-minute observation period. Consultation with an allergist to discuss risks/benefits may also be considered.
- Anyone with known and proven IgE-mediated reactions to polyethylene glycol or polysorbate are currently advised to avoid the Pfizer and Moderna vaccines. Given the rarity of allergies to these ingredients, it is unlikely for anyone to have this known allergy, unless specifically evaluated by a board certified allergist and confirmed with prior skin testing.
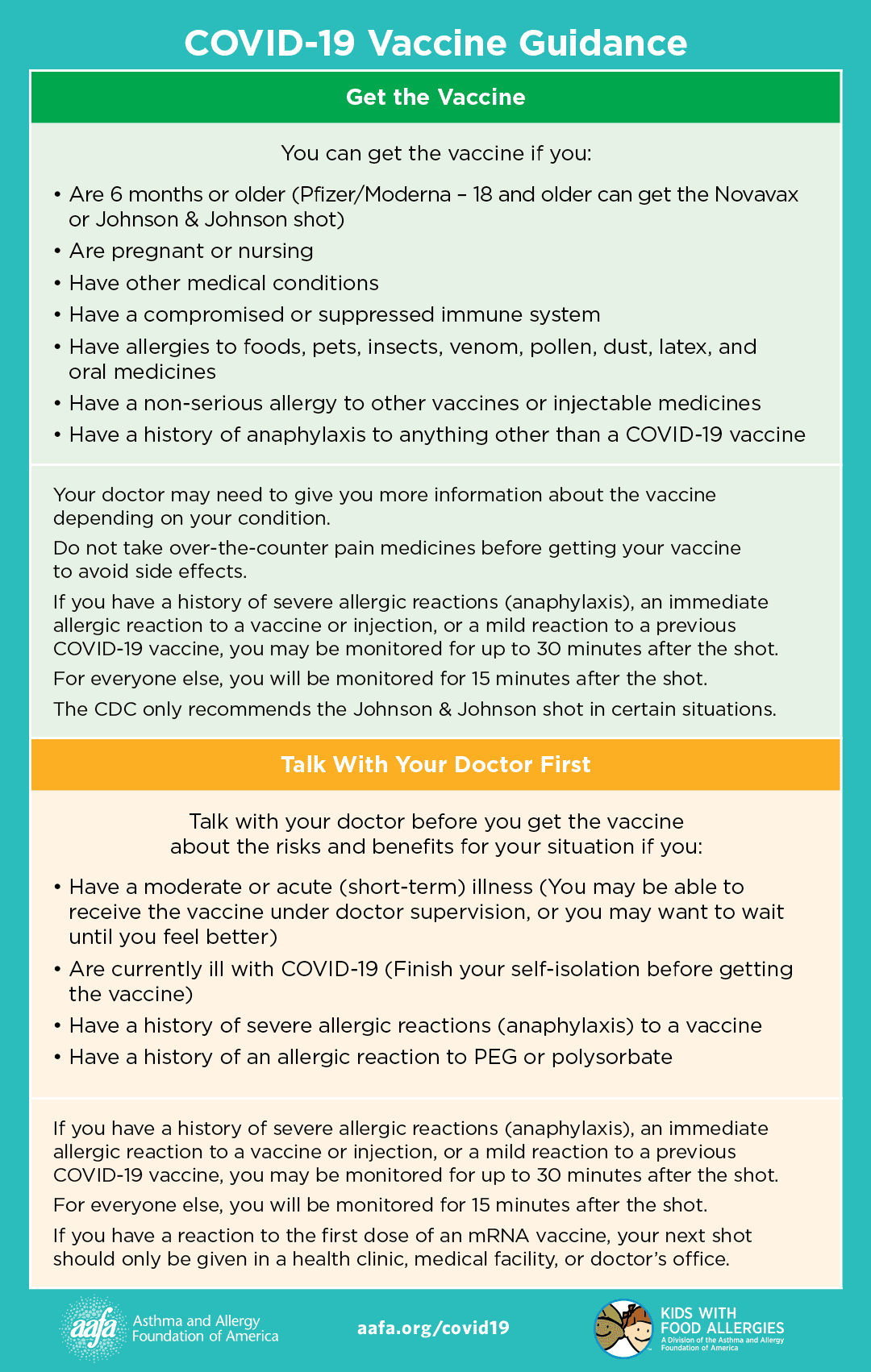
The Asthma and Allergy Foundation of America has developed a poster with this information, which may be useful for providers to share with their patients who have questions about asthma, allergies, and vaccines. The full version can be found here.